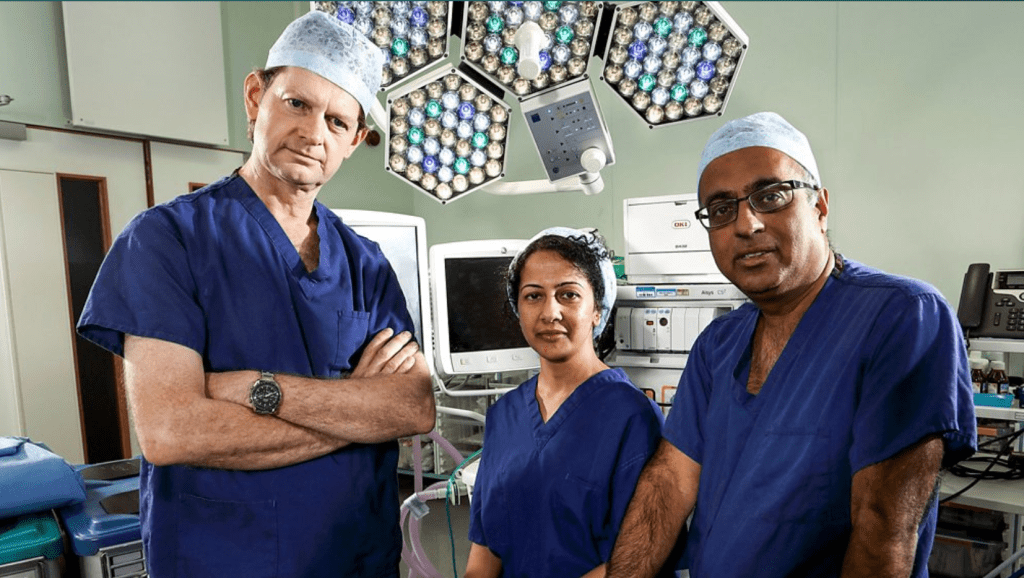
This is my personal review of Season 1 of the must-see BBC documentary series “Surgeons: At the Edge of Life”.
The series website is found at URL https://www.bbc.co.uk/programmes/b09m60sk
The series is a few years old and I remember watching in complete awe when it first broadcast on television. I am revisiting the episodes now as I try and gain a greater insight into the medical profession. The content is so interesting that I would like to share it on this website.
The first season begins with an introduction stating that the UK national health service (NHS) implements around 3 million (!) major operations each year. This is for a population of 67 million. Patients who undergo these, often very long, operations cannot imagine the levels of preparation required by the surgeons, the number of healthcare personnel required to assist during the operation and the critical decisions that need to be taken during each phase. All this happens while the patients are under the effect of anesthesia.
All three episodes are filmed at the Queen Elizabeth hospital in Birmingham where the 43 operating theatres witness operations that can be experimental, at the cutting edge of medicine.
One of the surgeons states that pushing the body to its limits comes with great risks to both patients and surgeons.
An operation will go wrong for a 30 second lapse of concentration.
Also, given the complexity of how different parts of the human body interact, each session comprises of
…lots of little operations bolted together. [It’s] physically and mentally extremely tiring.
Indeed, throughout the series it becomes very clear that patients place great trust in the work of the surgeon. The latter ultimately relies on teamwork, respect and trust in their colleagues.
I wholeheartedly recommend readers to watch this series. It is available on the BBC website and iPlayer apps and it doesn’t age: the commitment, knowledge and determination of the surgeons is a credit to the NHS staff involved and the very concept of our health service.
Patients need not concern themselves with the details and complexity of the actual operation; they are in the hands of an équipe of professionals performing small miracles on a daily basis to save and/or improve lives.
Episode 1 – The longest day
The first patient is a 53 year old woman with a fast-growing tumour in her upper jaw area. The removal of the tumour requires loss of her top jaw and one of the eyes.
The surgeons use a 3D software simulation based on CT scans to determine the exact measurements of the tumour area. This is part of the preparatory work that precedes the actual operation. The model serves to inform the surgeons of the dimensions of the replacement for the hollowed out part of the face, which in this case is made up of a small flap of bone and muscle cut from the woman’s hip.
The two principal surgeons had to work as a team to cut the hip part using precise measurements and attach it to the patient’s face!

The second patient was a 50 year old woman who elected to have a double mastectomy following multiple courses of treatment for an early form of breast cancer.
I always imagined that following removal of the breast tissue, an artificial breast would be inserted but in this episode, the surgeons used two flaps of skin and fat cut from the patient’s abdomen.
As one of the surgeons stated:
Everything about our bodies is important to our sense of self.
In the case of the female patient, the reconstruction of her breast following the mastectomy would ensure that her sense of being and femininity would be preserved.
Both sets of surgeons succeeded. As the episode title suggest, the operations were very long and complex. I became very aware of the sheer stamina required by the surgeons and team members.
Episode 2 – Last Chance Saloon
As the title suggests, both of the main operations featured in this episode referred to scenarios that would normally be inoperable. Only because of the latest advances in technology, the surgeons featured in this episode were even able to consider operating.
The first patient was a rather frail-looking 71 year old lady with a sarcoma – a rare cancer that develops in the bones and soft tissues, including fat, muscles, blood vessels, nerves, deep skin tissues and fibrous tissues.
As stated in the programme, sarcomas can grow to huge sizes. The patient had noticed swelling in her stomach; in a relatively short period of time, the cancer had grown from her ribs to her pelvis, crushing and displacing her anatomy in the process.
The surgeons didn’t know if the sarcoma could be removed prior to the operation. As the episode unfolded, the sheer size and weight (I believe 20Kg was mentioned) became evident. The effort required to cleanly remove the cancer was mind-blowing.
Equally amazing was the work required on the second patient, a 67 year old man with an advanced tumour, which had evolved from one kidney to the surrounding blood vessels and was making its way along a major vein called inferior vena cava (IVC).
The operation was required because had the tumour spread to the nearby heart, the patient could have died in very short time. Moreover, chemo- and radiotherapy had not worked.
The sequence of the operation involved removal of the kidney, stopping the heart (!), draining the blood and removal of the tumour after slicing open the the vein. During this period, the patient would be technically dead.
The method by which the heart can be stopped in a safe manner involves the cooling of the body to a much lower temperature (as if the patient was in hibernation). Cool cells require less oxygen.
The film footage of the work around the heart, the incision, the ‘bypass’ and the restart sequence was phenomenal.
Episode 3 – The Pioneers
This episode showcases some of the clinical trials taking place at the hospital.
Today’s research is tomorrow’s standard of care.
The trials are part of the NHS’s quest to deliver better outcomes for patients but they are inherently risky because the treatments are not proven. The trade-off is that if a particular trial is successful, the patient will benefit immediately; moreover, future patients will also benefit from the knowledge gained during the trial.
Patients must be fully informed of the trials’s potential benefits and risks; ultimately the patient must be absolutely sure they want to participate.
One of the episode’s patients was a female patient who had lived with liver cancer for the past 30 minutes, undergoing various treatments. She was awaiting a liver transplant.
For a liver to be eligible for transplant, it must pass a number of ‘quality’ checks. 400 livers per year are rejected, adding to general scarcity of livers for transplants.
The hospital is trialling a process called perfusion – a ‘sub-standard’ donated liver is placed in a machine that mimics the operation of the human body. Thus, over a <4 hour period, the liver is kept at body normal temperature and supplied with blood, oxygen and nutrients. At the end of the perfusion, the liver is checked to see if it’s suitable for transplant.
This process allows livers that would have in the past been rejected to be ‘recycled’ and used in operation. The episode showed the result of the perfusion and the time-sensitive operation that followed to actually transplant the liver.
A second patient was a 63 year old partially deaf man, who volunteered to take part in a trial to replace his external hearing aid device with a more discreet internal microphone. This operation, although not critical to the man’s lifespan, would potentially improve his quality of life since the current bulky hearing aid would no longer be needed.
The operation involved a canal drilled into the man’s skull, in the proximity of very important nerves: the one controlling facial movements and the one providing the sense of taste.
The implant initially failed the test since it was not picking up sound but a quick reconfiguration of the speaker apparatus resulted in a positive test and the operation could be completed.



Leave a reply to Review of 999: Critical Condition – Meddie Cancel reply